High-Pressure Oxygen Activates "Dormant" Neurons ("Idling" Neurons)
2025-07-31
A case study from 12 years ago involving a near-drowning incident was documented in the literature. By combining SPECT imaging with hyperbaric oxygen therapy (HBOT), areas of cortical hypometabolism were identified. Delayed imaging after a single HBOT session (1.5 ATA for 1 hour) suggested the presence of viable but metabolically sluggish neurons. After 80 HBOT sessions, the patient exhibited significant improvements in cognitive and motor functions. These findings support the hypothesis that dormant neurons and the ischemic penumbra can be reactivated when sufficient oxygen is supplied.
Thus, changes in tracer distribution following a single HBOT session may serve as a reliable prognostic indicator for viable neurons. Combining HBOT with physical and rehabilitation therapy may help sustain the permanent activity of reactivated dormant neurons.
Reference:
Neubauer RA, Gottlieb SF, Miale A Jr. Identification of hypometabolic areas in the brain using brain imaging and hyperbaric oxygen. Clin Nucl Med. 1992 Jun;17(6):477-481.
Case Details
A 15-year-old girl who had suffered a near-drowning accident at age 3 was brought to a hyperbaric center by her parents after hearing about HBOT. The parents were informed about the imaging and HBOT techniques (approved by the center’s advisory board) and provided informed consent.
The patient underwent sequential I-123 IMP SPECT imaging. Between two initial scans conducted 4 hours apart, she received a single HBOT session (1.5 ATA, 1 hour) in a Vickers monoplace chamber. Before the SPECT scan, Lugol’s iodine solution was administered to block thyroid uptake of free radioactive iodine. Subsequently, 4.2 mCi of I-123 IMP was injected intravenously. Imaging began 15–20 minutes post-injection using a Philips rotating gamma camera with an ADAC ARC 3300 computer, acquiring 64 frames (40 seconds each) over 45 minutes.
Prior to SPECT, MRI was performed using a Diasonics MT/S system (0.35 Tesla).
Results
·MRI showed moderate diffuse central brain atrophy with secondary hydrocephalus but no significant parenchymal lesions.
·Baseline SPECT (Fig. 1A) revealed reduced tracer uptake in the right parietal and temporal lobes, indicating hypoperfusion or hypometabolism.
·Post-HBOT delayed scan (Fig. 1B, 4 hours later) showed tracer filling in these previously hypometabolic areas.
·Repeat scans after a 2-month interval (no HBOT) demonstrated mild improvement in tracer uptake compared to the initial scan (Fig. 2), but delayed imaging under normobaric air (Fig. 3) showed minimal redistribution, unlike the significant post-HBOT changes.
·After 12 HBOT sessions, a follow-up scan (Fig. 4) appeared nearly normal, with only subtle hypometabolism in the right parietal cortex.
·Final scan after 61 HBOT sessions showed near-normal tracer distribution bilaterally, with no evidence of hypometabolism.
Clinical Relevance
Before the accident, the child had normal development (sitting at 6 months, walking at 9 months, speaking at 1 year). Post-accident, she remained comatose for 15 months and later exhibited intellectual impairment, requiring leg braces and a wheelchair.
Pre-HBOT psychological testing (Peabody Picture Vocabulary Test, Vineland Social Maturity Scale) indicated severe motor and social deficits but preserved higher cognitive potential (93rd percentile in vocabulary).
After 52 HBOT sessions, testing in English (previously Spanish) showed faster task completion and improved associative learning. Final evaluation noted:
·Clearer speech (especially in English).
·Increased alertness and attention span.
·Improved problem-solving speed and judgment.
·Better motor coordination (e.g., standing longer, climbing stairs with assistance).
·Neurological consultation confirmed these improvements, recommending further HBOT.
Discussion

The data suggest that I-123 IMP SPECT combined with HBOT can identify viable but dysfunctional neurons. Post-HBOT tracer uptake (Fig. 1B) exceeded redistribution effects seen under normobaric air (Fig. 3), supporting oxygen-induced reactivation of dormant neurons.
Potential mechanisms include:
·Enhanced oxygen diffusion overcoming metabolic deficits.
·Reversal of pH imbalances or edema-related diffusion barriers.
·Permanent neuronal reactivation after prolonged HBOT (Fig. 4).
·Prior studies align with these findings:
·Astrup et al. emphasized oxygen availability over blood flow.
·Ingvar, Lassen, and Saltzman reported neurological improvements with HBOT in stroke/ischemia.
·Animal models show HBOT increases survival post-stroke.
Conclusion:
HBOT + SPECT can detect metabolically dormant neurons in CNS injuries. Single-session HBOT-induced tracer redistribution may predict neuronal viability, while long-term HBOT + rehabilitation may sustain functional recovery. This case underscores HBOT’s potential in reactivating idling neurons, warranting further research in neurorehabilitation.

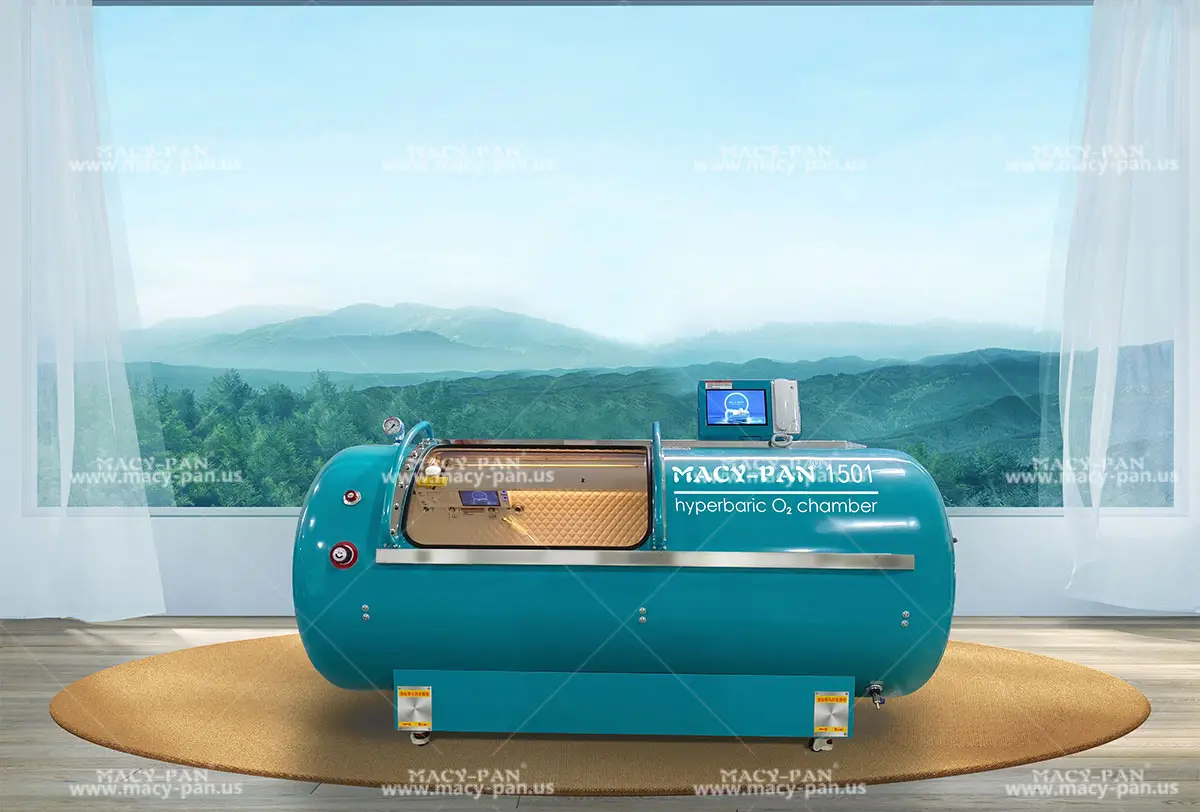
Hey, I’m Macy-Pan
1# Hyperbaric Oxygen Chamber Manufacturer in China. 18 years of industry experience. 126 countries and regions reached