Hyperbaric Oxygen and Cancer: Friend or Foe?
2026-02-05Can Cancer Patients Undergo Hyperbaric Oxygen Therapy?

As a hyperbaric oxygen physician, I often face questions from patients and colleagues: “Doesn’t hyperbaric oxygen ‘feed’ tumors, making them grow faster?” This reflects a common concern—after all, tumors need oxygen, and hyperbaric oxygen therapy (HBOT) involves breathing high concentrations of oxygen. Today, let’s explore the relationship between HBOT and cancer from a scientific and objective perspective.

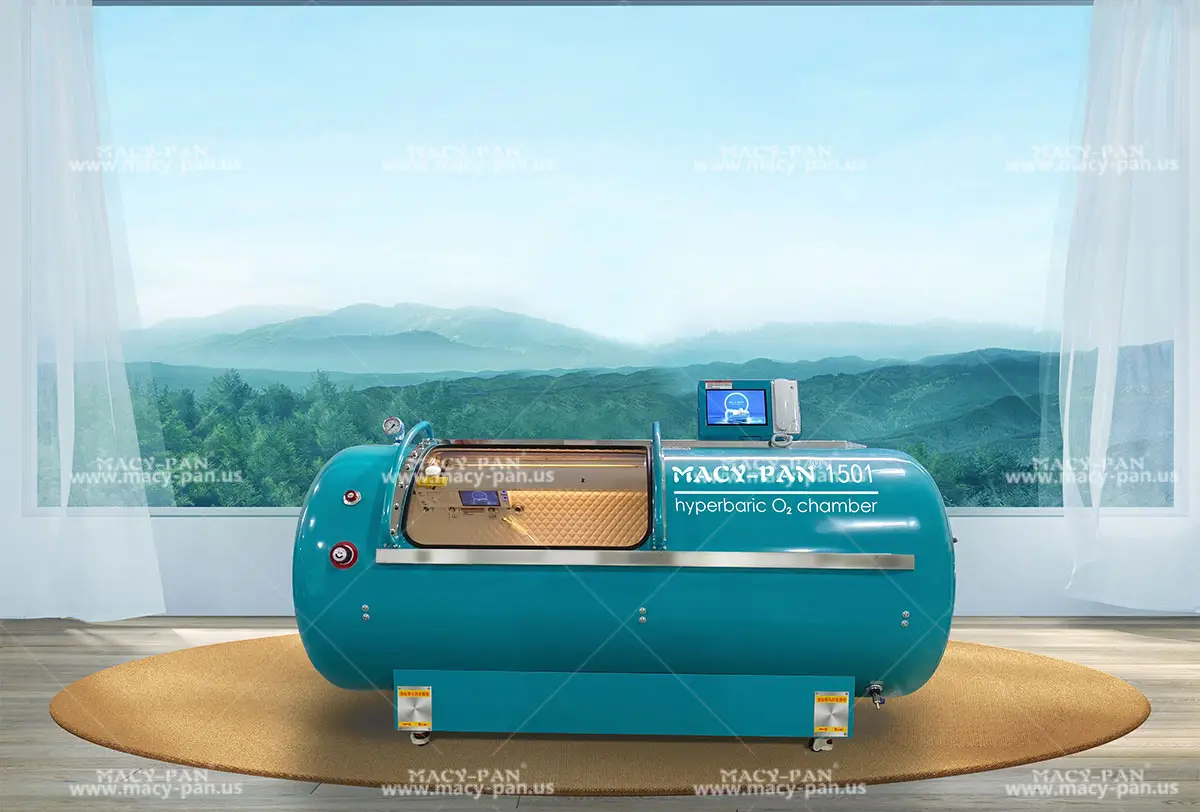
What Is Hyperbaric Oxygen Therapy?
First, a brief introduction to HBOT. This medical treatment involves patients breathing pure (or high-concentration) oxygen inside a pressurized chamber. Under pressures higher than normal, oxygen dissolves more readily in the blood and travels farther through tissues, significantly increasing tissue oxygen levels. It is a physical therapy that enhances tissue oxygenation independent of hemoglobin’s oxygen-carrying capacity. HBOT is commonly used to promote wound healing, treat carbon monoxide poisoning, decompression sickness, radiation-induced tissue damage, and more.
The Complex Relationship Between Tumors and Oxygen
Tumors do need oxygen to grow—as do all cells. However, as solid tumors expand, their blood supply often fails to keep pace, creating a hypoxic (low-oxygen) micro-environment in the tumor core. Hypoxia can lead to cell death, but some tumor cells adapt and survive. These surviving cells often become more aggressive.
How hypoxia increases tumor aggressiveness:
Hypoxia promotes the generation of oxygen free radicals in tumor cells, leading to DNA damage.
Hypoxia induces angiogenesis, stimulating tumor cells to secrete vascular endothelial growth factor (VEGF).
Hypoxia reduces apoptosis (programmed cell death) and may activate oncogenes or silence tumor suppressor genes.
Hypoxia shifts tumor metabolism toward glycolysis, reducing mitochondrial activity and further suppressing apoptosis.
Hypoxia drives tumor cells toward dedifferentiation, granting them stem cell-like properties and self-renewal ability.

How HBOT Affects Solid Tumors
- Direct Effects: Regulating Oxidative Stress and DNA Damage
HBOT increases reactive oxygen species (ROS), which are essential for cellular signaling. Its impact on tumors depends on its ability to modulate ROS balance: while elevated ROS may worsen DNA damage in tumors, HBOT can also enhance antioxidant defenses and improve mitochondrial function, potentially inhibiting tumor progression.
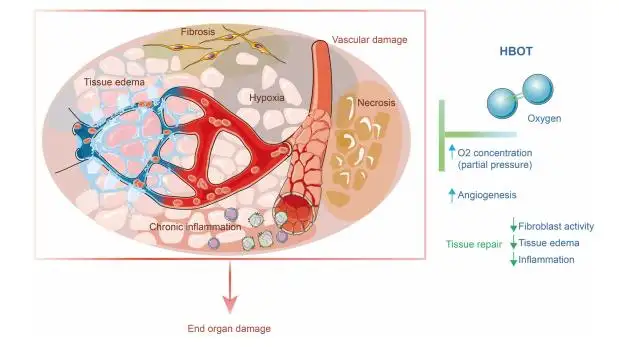
- Indirect Effects: Tumor Micro-environment, Angiogenesis, and Immune Regulation
The tumor micro-environment (TME) includes immune cells, blood vessels, extracellular matrix, fibro-blasts, and signaling molecules—all influencing tumor growth, spread, drug resistance, and recurrence.
HBOT raises tissue oxygen levels, down-regulates HIF-1α (a hypoxia-related protein), and increases susceptibility to ferroptosis, a form of cell death.
HBOT promotes normalization of tumor blood vessels and reduces collagen buildup, improving the TME’s acidic and high-pressure conditions.
HBOT alleviates hypoxia-related immune suppression, enhances T-cell infiltration and activation, and may help prevent recurrence.

What Does the Evidence Say?
The current international consensus in hyperbaric medicine is:
Standard HBOT doses (typically 2.0–2.5 atmospheres, 60–90 minutes per session) do not promote tumor growth or metastasis.
HBOT is not used to treat the tumor itself but rather to manage complications caused by cancer treatments (e.g., radiation injury, non-healing wounds).
For patients with active malignancies, HBOT requires careful evaluation by a multidisciplinary team, including an oncologist.
Clinical precautions:
Strict adherence to indications (e.g., radiation injury, chronic wounds).
Thorough risk-benefit assessment by both hyperbaric and oncology specialists.
Caution during active tumor progression or in highly vascular tumors.
Individualized treatment plans tailored to the patient’s condition.
In Summary
The relationship between HBOT and cancer is not as simple as “feeding” or “suppressing” tumors. In modern comprehensive cancer care, HBOT serves as a valuable adjuvant therapy to improve quality of life and manage treatment-related complications. The key lies in scientific evaluation, rational application, and multidisciplinary collaboration.
Medical progress is about balancing risks and benefits. For eligible cancer patients, HBOT can be a safe and effective option, helping them navigate their journey with greater stability.
HBOT also shows great potential in sensitizing tumors to treatment and managing radiation injury. Stay tuned for Part 2.
References:
1. Hachmo Y, et al. Hyperbaric Oxygen Therapy in Oncology: Current Evidence and Directions. Front Oncol. 2021;11:666240.
2. European Committee for Hyperbaric Medicine. Hyperbaric Oxygen Therapy in Cancer Patients: Clinical Guidelines. ECHM; 2017.
3. Youda, Meng,Liang, Zhou,Yong, Xia et al. Breaking the hypoxia barrier: Advances and challenges of hyperbaric oxygen therapy in cancer treatment.[J] .Biomed Pharmacother, 2025, 193: 118703.
Article reprinted from | Lai Huimin | Oxygen Stories |

Hey, I’m Macy-Pan
1# Hyperbaric Oxygen Chamber Manufacturer in China. 18 years of industry experience. 126 countries and regions reached