Hyperbaric Oxygen Promotes Fracture Healing in Patients with Pycnodysostosis
2025-08-07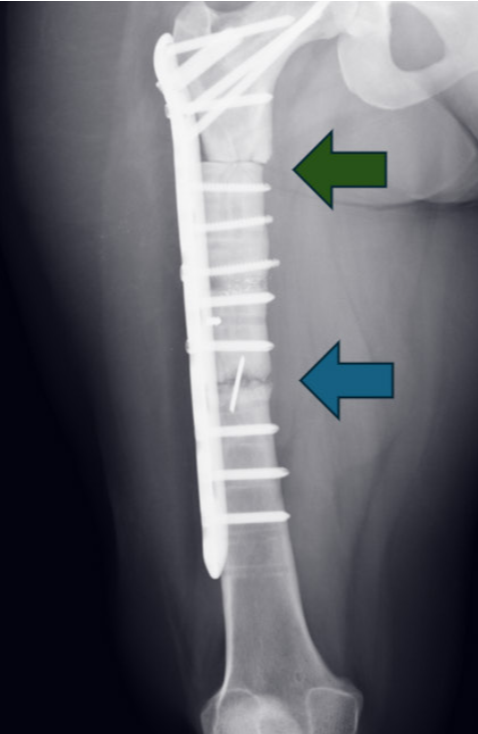
Pycnodysostosis is a rare lysosomal storage disorder characterized by short stature, craniofacial deformities, dental abnormalities, and increased bone fragility due to dysfunctional osteoclasts caused by mutations in the cathepsin K gene.
This case report describes a 43-year-old female patient with pycnodysostosis who experienced recurrent subtrochanteric femoral fractures and delayed bone healing despite multiple surgical interventions, including femoral osteotomy and bone grafting. Despite these measures, bony union was not achieved.
The patient underwent 39 sessions of hyperbaric oxygen therapy (HBOT). Post-treatment radiographs showed significant fracture healing, with continued improvement one month after treatment completion. The visual analog scale (VAS) pain score decreased from 4 to 1, and quality of life (SF-36) improved. HBOT enhances tissue oxygenation, stimulates osteogenesis, angiogenesis, and immune responses while optimizing osteoclast function, making it a promising approach for managing fracture complications in pycnodysostosis.
Reference:
Canarslan-Demir K, Yel AK, Aydin G, et al. Healing fragile bones: a case report on hyperbaric oxygen therapy in pycnodysostosis. Diving and Hyperbaric Medicine. 2025,55(2):191−194.
Patient Information
A 43-year-old patient with a prior diagnosis of pycnodysostosis had undergone surgery for a right femoral shaft fracture. Initial treatment involved open reduction and internal fixation with plate and screws. Fifteen years later, due to bone deformity, revision surgery was performed. However, bony union was still not achieved. One year after the revision, the patient sustained another traumatic fracture proximal to the initial fracture site and underwent surgery again. The same procedure was performed, but bony union remained elusive. Nine months later, a bone graft was performed to address the issue.
During the first evaluation in our department (two years after the revision surgery), the patient reported hip pain during movement, with a VAS score of 4/10, and reduced hip mobility. Computed tomography (CT) and X-ray imaging revealed a subtrochanteric fracture line with bone grafting, a femoral shaft fracture line, a plate, and 16 screws.
Hyperbaric Oxygen Therapy (HBOT)
The patient underwent HBOT (2.4 ATA, 120 minutes per session, once daily, five times per week, totaling 39 sessions).
No complications or adverse effects related to HBOT were observed.
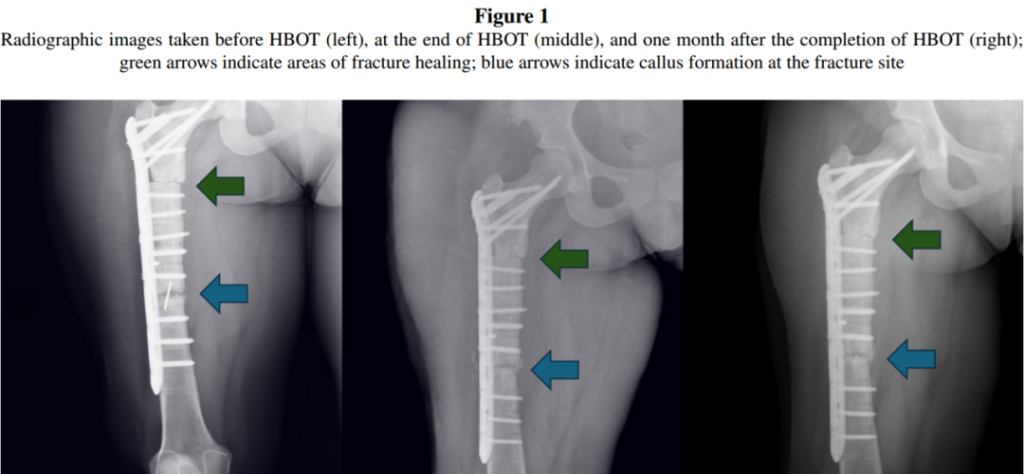
X-rays taken after the 39th HBOT session showed callus formation at the distal fracture site. Additionally, X-rays taken one month after completing HBOT demonstrated healing of the proximal fracture line (Figure 1). The patient’s hip pain (measured by VAS) decreased from 4 to 1.
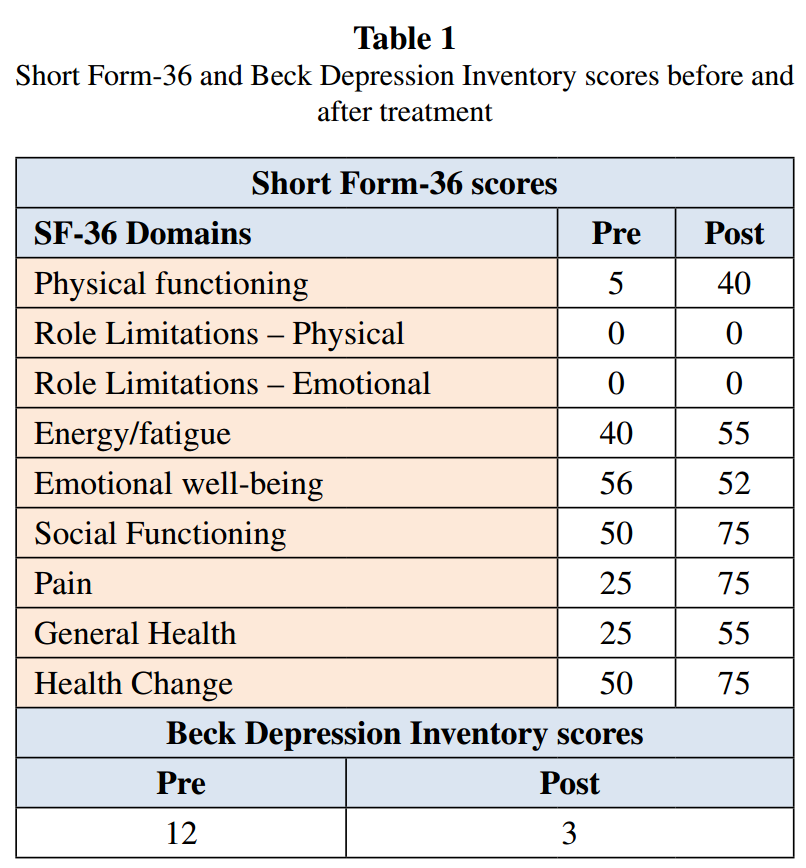
The Short Form Health Survey (SF-36) and Beck Depression Inventory (BDI) were administered before and after treatment (Table 1). Four months post-treatment, the patient reported no further fractures or pain.
Discussion
Pycnodysostosis is a rare lysosomal storage disorder characterized by short stature, acroosteolysis of the distal phalanges, craniofacial deformities (e.g., midface hypoplasia, prominent nasal bridge, frontal bossing, and micrognathia), dental abnormalities, osteosclerosis, and increased bone fragility. The pathogenesis of pycnodysostosis is linked to mutations in the gene encoding cathepsin K, located on chromosome 1q21. Cathepsin K is a crucial lysosomal cysteine protease that plays a key role in bone resorption and remodeling by degrading bone matrix proteins (such as types I and II collagen, osteopontin, and osteonectin) under low pH conditions. Deficiency of this enzyme leads to osteoclast dysfunction, resulting in impaired degradation of bone matrix proteins and abnormally fragile bone structure.
Pycnodysostosis is considered a rare disease, with an estimated prevalence of approximately 1 to 1.7 per million. Patients are typically diagnosed in childhood due to delayed closure of the anterior fontanelle or short stature. However, in adulthood, they often seek medical attention for recurrent fractures (especially long bone fractures, usually caused by low-energy trauma). As observed in our case, impaired fracture healing is a major challenge in managing pycnodysostosis, and there is no consensus on the optimal treatment approach. While surgical methods are primarily favored, conservative management has also been employed in specific cases.
This case report highlights the challenges associated with long bone fracture healing in pycnodysostosis and explores the potential benefits of HBOT in overcoming these difficulties. The hallmark of pycnodysostosis is defective bone resorption due to osteoclast dysfunction, leading to increased bone fragility. This condition predisposes patients to frequent recurrent fractures (spontaneous or due to low-energy trauma) and delayed healing.
In our case, multiple surgical interventions were performed to address recurrent subtrochanteric femoral fractures, osteotomy, and non-union. However, none of these procedures achieved bony union. This outcome aligns with the underlying pathophysiology of pycnodysostosis, where osteoclast dysfunction disrupts the bone remodeling process, significantly increasing the risk of non-union.
After 39 HBOT sessions, radiographic evaluation showed healing at the distal femoral fracture site, with further healing observed at the proximal fracture site one month later. Additionally, HBOT was associated with a reduction in the patient’s VAS pain score, improved quality of life (as assessed by the SF-36), and enhanced emotional state (as measured by the Beck Depression Inventory).
HBOT involves administering 100% oxygen to the patient in a hyperbaric chamber at pressures higher than normal atmospheric pressure. This process enhances oxygen delivery to partially ischemic or hypoxic tissues, stimulating oxygen-dependent leukocyte activity through the production of reactive oxygen species (e.g., hydrogen peroxide and superoxide). Furthermore, the hyperoxic environment promotes osteogenesis and supports angiogenesis, facilitating the replacement of damaged tissue with healthy bone. The improved vascular network allows better infiltration of immune cells, antibodies, and antibiotics into the affected area. Additionally, HBOT aids in clearing bone debris by optimizing osteoclast function.
HBOT appears to have contributed significantly to this patient’s recovery. Numerous studies have demonstrated that HBOT supports fracture healing histologically and radiographically, accelerates callus formation, increases bone mineral density, and enhances osteoblast activity and angiogenesis. Moreover, recent research suggests that HBOT may support bone healing in refractory orthopedic conditions, such as avascular necrosis of the femoral head, by halting disease progression and reducing the need for surgical intervention. Given the high metabolic activity of osteoblasts and osteoclasts, they are highly oxygen-dependent. HBOT enhances tissue oxygenation, providing the necessary oxygen to these cells, potentially boosting their activity. This process supports new bone formation and accelerates fracture healing. Thus, HBOT facilitates early fracture healing and positively influences the balance between bone formation and resorption. These mechanisms suggest that HBOT may serve as a potential therapeutic option for addressing complications such as non-union in pycnodysostosis patients.
Importantly, no complications or adverse effects related to HBOT were observed during the treatment. When implemented with appropriate protocols and monitoring, HBOT is a safe therapeutic modality.
In this case, the 39-session HBOT regimen was associated with a significant reduction in pain scores and marked improvement in quality of life (SF-36). The notable improvements in the "physical functioning" and "pain" subscales underscore HBOT’s potential benefits not only in pain relief but also in enabling patients to engage in daily activities and enhancing overall quality of life. These findings suggest that HBOT, as an adjunctive therapy, holds potential value in managing challenging fracture healing processes associated with conditions like pycnodysostosis.
While ideal, conducting controlled clinical trials for rare indications like this may not be feasible. Nevertheless, this report highlights HBOT as a potentially useful adjunctive therapy for fracture healing in pycnodysostosis patients. Other factors influencing bone healing in these patients, such as nutritional status, comorbidities, and genetic variations, must also be considered. The optimal HBOT protocol—including session frequency, pressure, duration, and combination with other treatments—remains unclear but, as mentioned, would be difficult to study.
In conclusion, this case report highlights the potential efficacy of HBOT in addressing impaired fracture healing in pycnodysostosis patients and underscores the need to explore novel therapeutic strategies for this rare genetic disorder.

Hey, I’m Macy-Pan
1# Hyperbaric Oxygen Chamber Manufacturer in China. 18 years of industry experience. 126 countries and regions reached