Medical Case Report: Hyperbaric Oxygen Therapy in Central Pontine Myelinolysis
2025-12-31Original by Song Xiangsheng, Renyi Hyperbaric Oxygen
A 51-year-old woman with a history of chronic alcohol abuse presented with dysarthria, dysphagia, hyperreflexia, and poor tandem gait. T2-weighted MRI revealed an oval-shaped hyperintense lesion within the pons.

A 10-day course of hyperbaric oxygen therapy (HBOT) completely resolved her symptoms. Follow-up MRI one year post-HBOT showed a significant reduction in the lesion size.
01 、Case Presentation
Patient: 51-year-old female
Chief Complaint: Difficulty walking and swallowing
Family History: Non-contributory
Past Medical History: History of alcohol use for over 10 years (daily consumption of 1000-1500ml of beer).
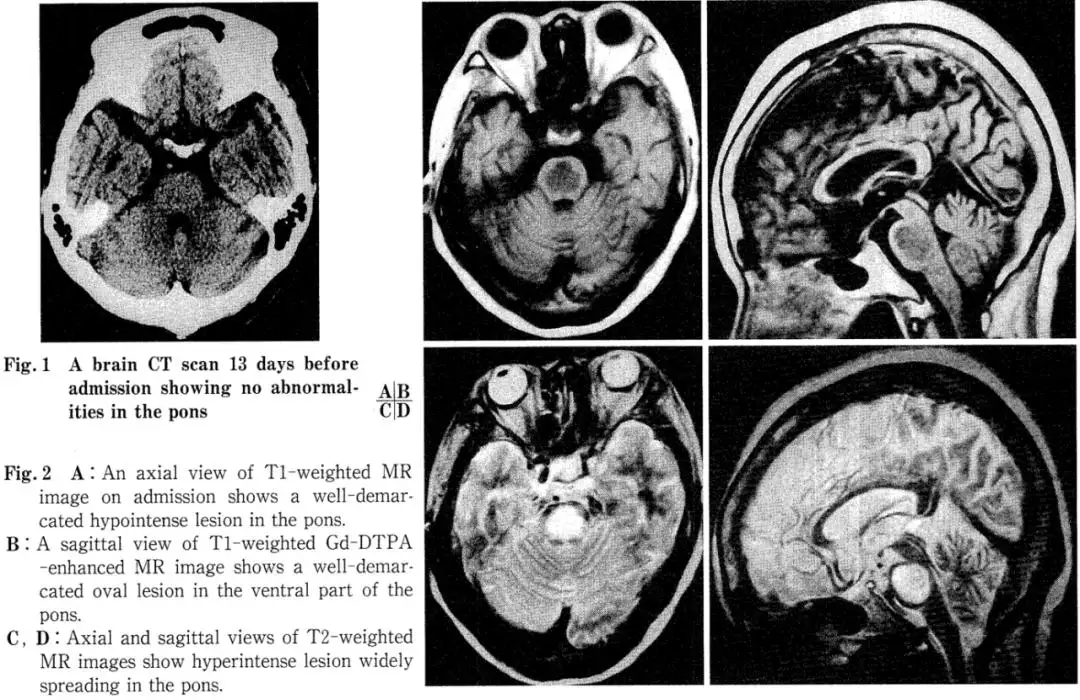
History of Present Illness: In mid-June 1998, the patient began experiencing episodes of transient visual darkening. By early July, she developed an unsteady gait and loss of taste sensation, leading to a visit to a local hospital on July 10. A CT scan at that time showed no abnormalities. However, as symptoms progressed to include dysphagia and dysarthria, she was admitted to our hospital on July 18 for further evaluation.
02 、Examination Findings
Physical & Neurological Exam on Admission: The patient was conscious with normal pupillary size, shape, and light reflexes, and had full extraocular movements. She reported diminished taste, right-sided tinnitus, and right-beating nystagmus. The gag reflex was diminished. She exhibited dysarthria and dysphagia consistent with pseudobulbar palsy. Although no pathological reflexes were noted, deep tendon reflexes were hyperactive in the lower extremities, and tandem gait was impaired. Blood chemistry revealed microcytic hypochromic anemia but no electrolyte abnormalities such as hyponatremia, hypoalbuminemia, or significant liver dysfunction.
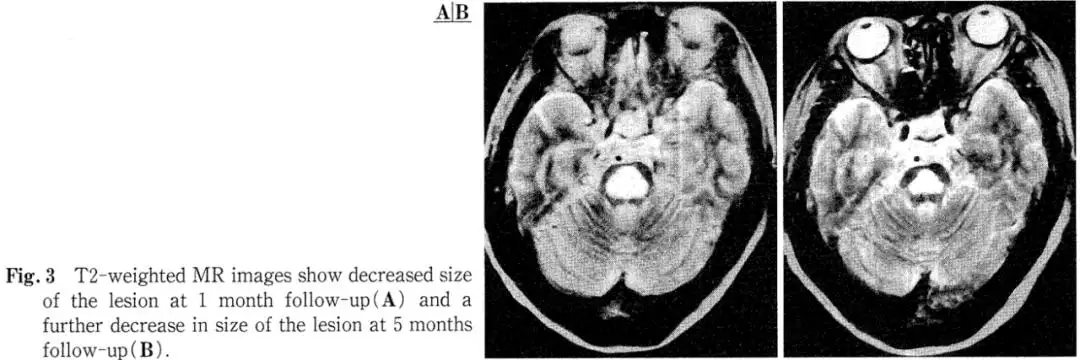
Imaging: A head CT performed at an outside hospital 13 days prior to admission was unremarkable (Fig. 1). However, admission MRI of the brain showed an oval, hypot intense area in the central pons on T1-weighted images, which appeared as a homogeneous hyper-intense lesion on T2-weighted images. This hypot intense area on T1 did not show enhancement after Gadolinium-DTPA administration (Fig. 2A-D). Follow-up MRI at 30 days and 5 months post-admission demonstrated a reduction in lesion size (Fig. 3A, B).
03 、Treatment and Outcome
Hospital Course: Considering potential diagnoses of brainstem infarction or multiple sclerosis, acute-phase HBOT was initiated at 2 atmospheres absolute (ATA) with pure oxygen. Within one week of starting HBOT, her taste disturbance and tinnitus improved. Dysphagia, dysarthria, and gait disturbance resolved almost completely within three weeks.
After completing a total of 7 HBOT sessions, the patient developed generalized hyperesthesia following a bath. Given the similarity to the "hot bath effect" seen in multiple sclerosis, she was treated with oral prednisone (15mg/day for one week, followed by 10mg/day for two weeks). She was discharged approximately one month later with no residual neurological deficits.
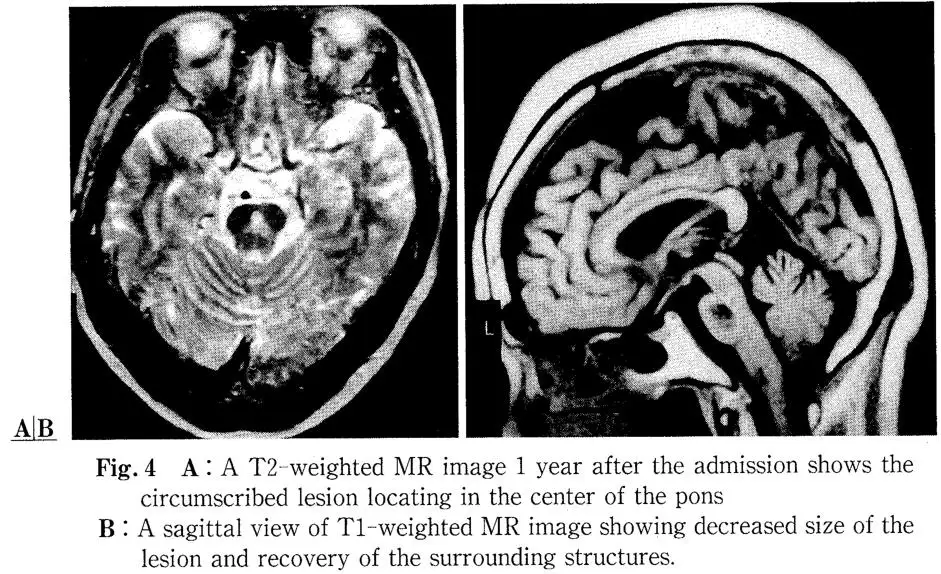
Follow-up: A brain MRI performed one year later showed further significant shrinkage of the pontine lesion (Fig. 4A, B), and neurological examination remained normal.
04、 Discussion
In 1959, Adams et al. reported four cases of alcohol-dependent patients who presented with pseudobulbar palsy and quadriparesis and died early in the disease course. They described the pathohistological hallmark: a centrally located pontine lesion with myelin destruction but relative preservation of neurons, axons, and blood vessels, coining the term "central pontine myelinolysis" (CPM).
Regarding etiology, Adams et al. initially postulated a deficiency state due to exogenous or endogenous intoxication. Since then, cases have been reported not only in chronic alcoholism but also in malnutrition, hyponatremia, and notably, following its rapid correction. Recent reports also include CPM after pituitary tumor surgery and hemodialysis. In cases like ours without documented hyponatremia in an alcoholic patient, underlying metabolic disturbances are suspected, though a definitive cause remains elusive in this discussion. Notably, Western literature reports CPM incidence as high as 15% post-liver transplantation, highlighting it as a potential complication of organ transplantation requiring attention in Japan as well. Furthermore, autopsy studies revealing asymptomatic CPM suggest the condition is not rare, and its detection is expected to increase with more widespread use of brain imaging.
The pathophysiology of CPM, while not fully proven, is thought to involve rapid serum sodium shifts or hyperosmolar states causing osmotic endothelial injury, which becomes an attack factor for myelin, triggering vasogenic cerebral edema.
Neurologically, spastic quadriparesis, lower cranial nerve palsies, and pseudobulbar palsy are the main reported features. In this case, we attribute the hypogeusia to involvement of gustatory pathways, and the tinnitus, nystagmus, and gait ataxia to vestibular nucleus dysfunction. The post-HBOT generalized paresthesia was likely due to medial lemniscus involvement. Thus, clinically, a widespread pontine lesion was suspected, which was corroborated by MRI.
Regarding imaging findings, most reported MRI features of CPM show hypot intensity in the central pons (sparing the tegmentum) on T1 and hyperintensity in the same region on T2. Koch et al. noted that the characteristic MRI feature of CPM is an oval-shaped lesion in the sagittal plane, typically sparing the pontine tegmentum and ventrolateral areas. In our case, the tegmentum and corticospinal tracts were also spared.
Furthermore, Thompson et al. suggest that as myelin lipid protons do not significantly affect MRI signal, acute demyelination alone may not cause the observed changes. The signal alterations are primarily attributed to edema. These changes may evolve into gliosis in the chronic phase, partly explaining the minimal changes on follow-up MRIs in some cases.
Conversely, sequential MRI often shows that acute-phase lesions rarely shrink or disappear completely, with most persisting for 6 months to 2 years. Miller et al. reported one case where the pontine abnormality decreased in size after six months, while another showed no change. In our patient, shrinkage was evident on the one-month follow-up MRI, and the lesion was reduced by more than half after one year. Therefore, long-term MRI observation in CPM is considered to reflect acute-phase edema, subacute-phase demyelination, and chronic-phase gliosis, which is crucial for differential diagnosis. From this perspective, CPM's MRI appearance can mimic cerebral infarction, metastatic or glial tumors, multiple sclerosis, encephalitis, and post-chemoradiation changes. Differentiation from tumors is based on the lack of mass effect; from multiple sclerosis by the larger, solitary lesion; and from infarction by the sparing of corticospinal tracts. However, as Kleinschmidt-DeMasters et al. also reported in 8 autopsy-confirmed asymptomatic CPM cases—all featuring small central pontine lesions—and as Koch et al. emphasized, differentiation from infarction can be most challenging, underscoring the importance of clinical context and sequential MRI observation.
Additionally, while most reported cases, including ours, show no Gd-DTPA enhancement, Koch et al. reported a case with symmetric central pontine lesions demonstrating ring-like peripheral enhancement. They proposed a mechanism similar to that in multiple sclerosis: transient blood-brain barrier disruption at the interface between demyelinated lesions and normal brain. Furthermore, while lesion size often correlates with clinical severity, our patient showed rapid neurological recovery after initiating HBOT despite a large initial lesion sparing only the pontine margins. This is more easily understood if the acute pathology is primarily edema.
Finally, there are scarce reports on specific treatments for CPM, with management primarily focused on the underlying condition. While steroid pulse therapy has been reported as effective, to the best of our knowledge at the time of writing (1999), there were no published case reports on HBOT for CPM. HBOT is considered beneficial for cerebral infarction, and our institution has observed positive outcomes in minor stroke cases. Although the exact mechanism remains unclear, HBOT is also reported to be effective for cerebral edema associated with various conditions. Therefore, if the acute phase of CPM is indeed characterized by edema, HBOT may hold promise as a future therapeutic intervention for CPM.

Hey, I’m Macy-Pan
1# Hyperbaric Oxygen Chamber Manufacturer in China. 18 years of industry experience. 126 countries and regions reached